Just as you would want to cure a painful skin condition or sore joint in your pet, consider relieving pain in your pet’s mouth. When an oral problem is caused by poorly aligned teeth, orthodontic treatment may be needed.
Orthodontics for pets is not frivolous and is seldom performed for cosmetic purposes. Orthodontic procedures are the tools used to improve dental function and reduce pain.
Just as you would want to cure a painful skin condition or sore joint in your pet, consider relieving pain in your pet’s mouth. When an oral problem is caused by poorly aligned teeth, orthodontic treatment may be needed.
Orthodontics for pets is not frivolous and is seldom performed for cosmetic purposes. Orthodontic procedures are the tools used to improve dental function and reduce pain.
Teeth that are crowded, rotated, or tilted at abnormal angles can result in:
- Early onset and increased severity of oral (mouth) infection.
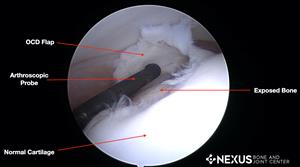
- Damage to the soft tissues of the mouth from sharp teeth penetrating the unprotected gum and mouth tissues. Lower teeth can actually poke holes through the hard palate, causing food to be packed into the nasal cavity! Excessive wear: when abnormally aligned teeth grind against each other, the abrasion frequently wears through the enamel, causing the weakened tooth to fracture so that the nerve becomes exposed.
- Pain in the jaw joints as well as in the gums, lips, cheeks, and teeth.
Genetic or Not?
Occlusion is the way in which teeth align with each other. Occlusion is controlled by genetics, nutrition, environment, and by mechanical forces generated by the interlock of the upper and lower teeth. Some abnormal bites (malocclusions) are genetically influenced, such as severe over or under bites and wry bites. Other bite abnormalities are known to be acquired (non-genetic). Acquired malocclusions can result from tug of war games played with towels or ropes that move teeth into an abnormal position. Traumatic birthing can also be responsible for some acquired abnormalities.
To help define whether the malocclusion is genetic in origin, interdigitation of the premolars is studied. In breeds that have medium and long muzzles, the premolars should meet in a saw toothed fashion. For example, the tip of the lower third premolar should be positioned equally between the crowns of the upper third and fourth premolars. If the tip of one premolar points to the tip of another premolar, there may be a genetically-induced malocclusion. This only holds true in breeds that do not have shortened muzzles.
Some genetic bite problems do not show up in each litter because they are passed on recessively. The goal of selective breeding is to mate one animal to another that has superior occlusion.
Retained Deciduous Teeth
Normally the root of the deciduous (baby) tooth is reabsorbed, making room for an adult tooth. Should this fail, the adult tooth may move from its normal position, resulting in malocclusion. The resulting double set of teeth overcrowds the dental arch, causing food to become trapped between the teeth, which lead to early periodontal disease. A double set of roots may also prevent normal development of the socket and erode periodontal support around the adult tooth, resulting in early tooth loss. A retained deciduous tooth should be extracted as soon as an adult tooth is found in the same area as the baby tooth. If the extraction is performed early, the abnormally positioned adult tooth usually moves to its normal location.
Some breeders trim or cut deciduous teeth in the hope that they will be shed early and prevent orthodontic problems. When the tooth is cut in half, pulp is exposed to oral bacteria causing infection, pain, and tooth loss. Unfortunately, the remaining infected root can interfere with the emerging adult tooth, which may not come in normally.
Dental Interlock
Jaws do not grow at equal rates. If deciduous (baby) teeth erupt during an accelerated growth phase of one jaw, both sets of primary teeth can interlock and result in an abnormal bite. Even genetically normal dogs can occasionally develop abnormal bites due to the interlock of primary teeth. If an under bite is noted before the permanent teeth erupt, treatment may be helpful. Removing the primary teeth (from the shorter jaw) that are interfering with the forward jaw growth may allow the upper jaw to lengthen unimpeded, if the procedure is performed by 10 weeks of age. This procedure, called interceptive orthodontics will correct about 50% of minor jaw length malocclusions by the time permanent teeth erupt. Extracting teeth does not stimulate jaw growth; it only removes a mechanical barrier to genetic control of the growth process.
Breeders, show judges, veterinarians, and others who wish to describe specific dental conditions in dogs and cats should use proper orthodontic terms. Over bite, open bite, over jet, level bite, overshot, under bite, anterior cross bite, posterior cross bite, wry bite, and base narrow canines are orthodontic terms that are confusing at times.
Missing or Extra Teeth
Dogs and cats may be born without the proper number of teeth. The overcrowding from extra (supernumerary) teeth can cause periodontal disease. The American Kennel Club sets acceptable standards for show dogs about the minimum number of teeth for each breed. Dental x-rays can be taken as early as 10 weeks of age to evaluate if the dog has the correct number teeth. X-rays are recommended as a part of the prepurchase examination in certain breeds. Missing teeth (hypodontia) usually occur in the premolar area, but any tooth in the mouth may not erupt. Missing or extra teeth are considered genetic faults. Collies and Doberman Pinchers are most commonly affected. Sometimes the missing tooth is trapped below the gum line, and a dental x-ray can be taken to determine if there is an unerupted tooth.
Misdirected Canine Syndrome
Misdirected canine syndrome is a bite abnormality where retention of the deciduous (baby) tooth tilts the erupting permanent canine tooth into an abnormal location. The opposing canines may not have room to occlude properly, resulting in abnormal wear, periodontal disease, or early tooth loss.
Occlusion
The way in which teeth align with each other is called occlusion. Normal occlusion in most medium and long muzzled breeds consists of the upper (maxillary) incisors that just overlap the lower (mandibular) incisors (scissors bite). The lower canine should be located equidistant between the corner (lateral) incisor and the upper canine tooth. Premolar tips of the lower jaw should point between the spaces of the upper jaw teeth.
Malocclusion
Malocclusion refers to an abnormal tooth alignment. Over bite (mandibular distoclusion, parrot mouth, over shot, class two, over jet, mandibular brachygnathism) occurs when the lower jaw is shorter than the upper. There may be a gap between the upper and lower incisors when the mouth is closed. The upper premolars are displaced at least 25% toward the front compared to the lower premolars. An over bite malocclusion is not considered normal in any breed and is a genetic fault. The most commonly affected breeds are those with elongated muzzles (Collies, Shelties, Dachshunds, and Russian Wolfhounds).
An underbite (mandicular mesioclusion, under shot, reverse scissors bite, prognathism, class III) occurs when the lower teeth protrude in front of the upper jaw teeth. Some short-muzzled breeds (Boxers, English Bull Dogs, Shih-Tzus, and Lhasa Apsos) normally have an under bite, but it is abnormal when it occurs in medium-muzzled breeds. When the upper and lower incisor teeth meet each other edge to edge, the occlusion is considered an even or level bite. Constant contact between upper and lower incisors can cause uneven wear, periodontal disease, and early tooth loss. Level bite is considered normal in some breeds, although it is actually an expression of under bite.
Rostral cross bite occurs when canine and premolar teeth on both sides of the mouth occlude normally, but one or more of the lower incisors are positioned in front of the upper incisors. This condition can be caused by tug-of-war games, retained primary teeth, or impacted roots. Anterior cross bite is a common malocclusion. It is not considered a genetic or inherited defect. Posterior cross bite occurs when one or more of the premolar lower jaw teeth overlap the upper jaw teeth. This is a rare condition that occurs in the longer nosed dog breeds. A wry mouth or wry bite occurs when one side of the jaw grows more than the other.
Wry bites show as triangular defects in the incisor area. Some of the incisors will meet their opposing counterparts while others will not. Wry bite is a severe inherited defect. Base narrow canines occur when the lower canine teeth protrude inward, often producing damage to the upper palate. This condition is either due to retained deciduous teeth, or by an overly narrow mandible. Base narrow canines may be corrected through orthodontic devices that push the teeth into normal occlusion. An open bite occurs when some incisors are displaced vertically and do not touch. The tongue will often protrude.
Rotated teeth, commonly affecting the upper third premolar, occur mostly in short-muzzled breeds. Selective breeding has created undersized mouths that cannot accommodate 42 teeth in normal alignment. The rotated tooth root closest to the palate is prone to periodontal disease. Strict tooth brushing may be helpful in saving a rotated tooth, but frequently it cannot be saved.
Orthodontic Care
Many abnormal bites can be corrected. Orthodontic care should be performed by veterinarians familiar with tooth movement principles. Sometimes breeders use rubber bands to move teeth but they compromise the gum tissue around teeth, leading to periodontal disease, pain, and early tooth loss. Orthodontic care should be reserved to ease pet discomfort by realigning teeth in those animals that will not be used for show. Tooth movement is accomplished by employing brackets, acrylic retainers, springs, and elastics. Fortunately, in animals orthodontic movement can usually be accomplished in months rather than years.
If your dog’s or cat’s teeth do not appear to meet normally, have your veterinarian take a peek and make recommendations to help your pet.