Breast Cancer Happens in Companion Animals
Print an 8.5″x11″ pdf of this poster.
Everyone reading this is a mammal (unless you are a particularly sentient anemone, coelacanth or axolotl), and one of the things that pegs us as mammals and unites us all is…well, boobs. Yes, even the men and boys. Boob-bearers, all of us.
Let me explain.
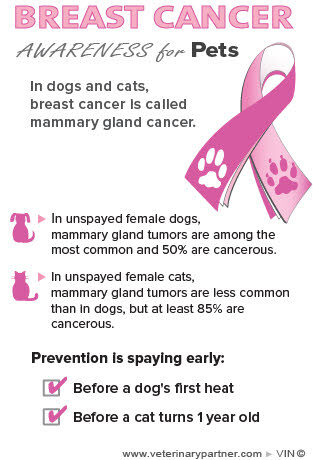
But it still seems to shock people to learn that dogs, cats, rabbits, rats and a host of other domestic species can get breast cancer, too. Since the aim of Breast Cancer Awareness Month is to raise awareness, our aim here is to wave the flag for those who can’t speak for themselves and raise awareness of mammary cancer in companion animals. We also want people to know that breast cancer and mammary gland cancer are the same disease; it’s just called by a different name in other species. Check out the poster we created for use in veterinary hospitals that we hope will help pet owners understand that they’re the same.As a pre-amble ‒ and the way this is going it could be a “pre-ramble” ‒ October is Breast Cancer Awareness Month.

I think people are fairly keyed in to the fact that humans can get breast cancer, or mammary cancer, as it is called in companion animals; its gnarled and potentially deadly hand has touched the lives of many of you, I presume. My own mother had surgery to have a tumor removed that was, luckily, low grade.
Some numbers may help to illustrate the risks to dogs and cats. For humans, breast cancer happens more frequently in more developed countries, and accounts for about 10 percent of all deaths in women between 20 and 59 (source: World Health Organization).
Data for dogs and cats and other domestic species are harder to come by as there is no World Doggy Health Organization database to be accessed as easily as WHO data, but estimates are that 1 in 4 dogs who are not spayed and experience more than one heat cycle will develop mammary tumors. Those stakes are high enough that Vegas would avoid this bet like the plague.
Happily, for dogs or cats who are spayed before they are sexually mature (the usual timeframe for a spay is before 6 months of age) mammary cancer is virtually unheard of. Learn more about the specifics of the disease and treatment in dogs and cats.
The terminology surrounding lumps, tumors and cancer can be a little daunting sometimes, and is often a source of confusion. One thing to keep in mind is that the word tumor does not always mean cancer. Cancer implies malignancy, or a predilection to grow rapidly and spread to other parts of the body: it’s a process known as metastasis, in which a tumor says, in essence, I’m outta here and decides to infiltrate new and exciting regions for growth. A tumor can be benign or malignant, but cancer is always malignant.

So how do we know which lump is bad, and which is not likely to be a problem for our pets? Sadly, there’s no easy way. Any lump found on a pet’s mammary gland has the potential to be cancerous, so having your veterinarian remove the lump (or a piece of it, in what is known as an incisional biopsy) and submit it for analysis is an important part of keeping your pets safe from this disease.
A biopsy is a piece of tissue that can be preserved and looked at under a microscope by a pathologist to determine what the lump is (mammary tissue vs. some other tissue that just decided on a whim to form a lump) and whether the lump is cancerous, or as doctors call it, malignant. You can’t tell if tissue is cancerous just by the way it looks, how it feels or where it is.
There is one intermediate step that can offer information to your veterinarian on how extensive or radical surgery to remove the lump should be. This is known as a fine needle aspirate, or FNA. With an FNA, you don’t get a piece of the mass, you just suck some cells up into the needle and place them onto a slide. It is much less invasive and doesn’t usually require any sedation or anesthesia, but the trade-off is that it is a less accurate test and less likely than a surgical biopsy to tell you the badness level of the tumor. An FNA is actually notoriously unreliable for mammary masses as far as predicting malignancy but can help make sure the lump is from mammary tissue and not something else that set up shop in the same area.
Medicine is often like that – the invasive stuff is the most accurate, and the easiest stuff gives you the least useable information. It’s like food where the good stuff tastes bad and the stuff that tastes great kills you. The universe can seem like a vast, cruel joke some days.
I know this sounds complex, intimidating and potentially invasive – not to mention expensive. The good news is that the take-home on this is pretty simple: spay your pet before she goes into heat, unless you have a rock-solid breeding plan for your purebred pet, and have your veterinarian check out any suspicious lumps. That’s about it. Luckily, your trusted family veterinarian has the skills and knowledge to guide you and your pet through this maze to ensure the highest degree of success.